Arthritis in the knee can be a challenging condition, impacting your daily life and mobility. As a physician, I’m here to provide you with a comprehensive guide to understanding the causes of knee arthritis, various treatment options, and steps you can take on your own to minimize and manage symptoms.
Understanding Knee Arthritis: Causes and Diagnosis
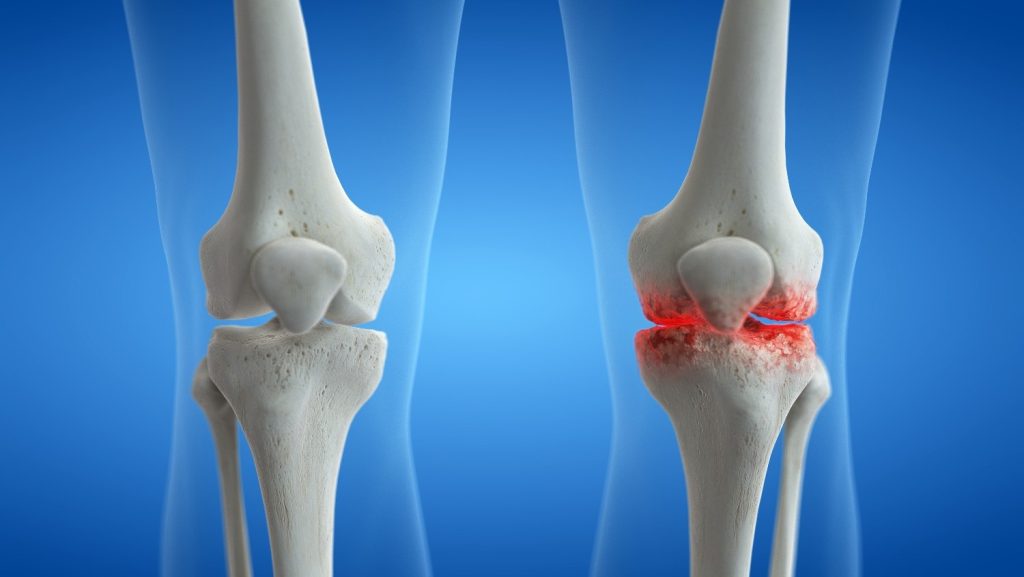
Knee arthritis is often the result of wear and tear on the joint over time, leading to the breakdown of cartilage. This can cause pain, swelling, and reduced flexibility. Additionally, inflammatory arthritis conditions, such as rheumatoid arthritis, can also affect the knee joint. Cartilage is like the tread on a tire. Your genetics determine that quality of the tire, but your lifestyle dictates how fast the cartilage breaks down. The more miles in a given time, the more quickly it wears out. Your driving style also affects how long the cartilage lasts. If you are significantly heavier, that is more pressure and friction on the cartilage which will lead to more rapid loss of cartilage. The pain you notice is due to the irritation and inflammation in the cartilage, either due to loss of volume or defects in the cartilage.
Diagnosing arthritis involves a thorough medical history, physical examination, and often imaging studies. X-rays are commonly used to assess joint damage, while MRI and CT scans provide detailed images of soft tissues and can help identify inflammation. Xrays indirectly show the space between the bones, but the actual cartilage and meniscus is a soft tissue that requires MRI to effectively see on imaging.
Treatment Options: Taking Control of Your Knee Health
1. Lifestyle and Diet Changes:
- Maintain a healthy weight to reduce stress on your knee joints.
- Adopt an anti-inflammatory diet rich in fruits, vegetables, whole grains, and omega-3 fatty acids. Avoid processed foods, refined sugars and trans fats as they trigger inflammation which may manifest as sore and achy joints (at least more than normal).
- Regular low-impact exercise, such as swimming or biking, can help maintain joint flexibility.
2. Exercise:
- Engage in exercises that strengthen the muscles around your knee, providing added support. (Search our blog for next week’s post to find a knee arthritis exercise regimen that you can implement).
- Low-impact activities like walking, yoga, and tai chi can improve joint function.
3. Over-the-Counter Treatments:
- Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen can help reduce pain and inflammation.
- Topical treatments, such as creams or patches, may offer localized relief. Some common over the counter topical creams include BioFreeze, IcyHot. My favorite is Voltaren gel, but it has to be applied 3-4 times per day for moderate arthritis.
- Braces – Knee braces can help stabilize the knee. 50% of patients have what is called one compartment arthritis. An example would be where the inside of the knee might be wearing down but the outside or kneecap is relatively spared. These patients may benefit from an unloader knee brace that puts pressure on the outside of the knee, relieving pressure on the inside of the knee. It takes a bit of trial and error to get the settings right but studies have shown that it can help delay surgery for more than 2 yrs on average.
4. Supplements:
- Glucosamine and chondroitin sulfate may help improve joint health. These safe and found in most stores and online.
- Omega-3 supplements have anti-inflammatory properties.
- There are a number of other supplements with research showing that they can modify inflammation, improve range of motion, and reduce the pain and soreness. That is why I created JointLife, an all in one super supplement. You no longer have to guess which supplement on the local store shelf is the best one to try. JointLife combines them all into a convenient 4 tablet daily serving size. You can find it at www.tryjointlife.com or www.bluefiresupplements.com.
Physician’s Role: Treatment Algorithm and Prescriptions
1. Medications:
- Prescription Analgesics and anti-inflammatories, like meloxicam, celecoxib, or naproxen can alleviate pain and inflammation. Tramadol can also help but merely masks the symptoms and is a controlled substance. If you have associated nerve pain (burning/tingling/numbness), then medications such as gabapentin and lyrica can help but sometimes the side effects are almost as bad the nerve pain.
- Disease-modifying antirheumatic drugs (DMARDs) may be prescribed for inflammatory arthritis, such as rheumatoid arthritis.
2. Injections:
- Corticosteroid injections can provide short-term relief by reducing inflammation.
- Platelet-rich plasma (PRP) injections promote healing.
- Hyaluronic acid injections act as a lubricant for the joint.
In-Depth Look at Injections: Benefits and Risks
- Corticosteroids: Effective for reducing inflammation but may have side effects like joint infection or thinning of nearby bone. Recent studies have shown that corticosteroids always accelerate the loss and thinning of cartilage. In trying to reduce the inflammation and pain, it has the effect of worsening the cause of the pain.
- PRP Injections: Extracts platelets from your own blood to stimulate healing. Risks are minimal, with potential benefits lasting several months. We all know that blood flow is require for healing. The problem with joints is that joints have a relatively poor blood supply, therefore the growth factors that normally repair and support healthy tissue are not available. With PRP, you are concentrating the cells which include exosomes and growth factors directly into a joint where they go to work and can benefit patient for months. PRP has been shown help maintain the joint, and prevent or slow down the further loss of cartilage for a time. Normally, when arthritis sets in, the inflammation actually promotes even more rapid loss of cartilage, so PRP can help maintain for a time. The main drawback is the cost as PRP injections can cost $500-1500 per injection and insurance is not covering it as of yet.
- Hyaluronic Acid Injections: Provide lubrication for the joint, offering relief for osteoarthritis. Risks include joint swelling or infection. It temporary “greases” the joint but there is no lasting benefit beyond a few weeks or 1-2 months. It is typically $1500 or more for a series of 3 injections, but depending on deductibles and coinsurance, insurance will typically cover them.
Surgical Options: Knowing When to Consider Them
When your arthritis symptoms affect your quality of life, despite changes in lifestyle, diet, exercise, supplements, prescriptions and injections, then the orthopedist will typically discuss surgical options. In their mind, they typically view arthritis as a terminal illness. It is viewed as a progressive degeneration of the joint, since you will continue to “put miles on the tires” so to speak and no matter what, the tread wears down with use as does our cartilage over time. We may hit a few potholes that create and accelerate damage, and often it is the culmination of the potholes and the miles that dictates when the arthritis negatively impacts our quality of life and forces us to do something. With the model of a terminal condition in mind, some orthopedists will recommend the options that I wrote about above, but others, who believe that you will inevitably end up on their surgical table, will recommend to skip all of those options as they figure you might as well let them replace the joint sooner, since it is an inevitability in their mind.
Stem Cells: The New Kid On The Street
This is a good time to briefly mention a new treatment causing a needed paradigm shift in our normal view of arthritis. Newer evidence and ongoing research continues to confirm that stem cell therapy can increase cartilage volume. In other words, MRI studies have shown that Mesenchymal Stem Cells can and lead to putting tread back on the tires. It is the only therapy to date that gets to the root cause of the problem, loss of cartilage, and addresses that as opposed to just managing the symptoms. Studies have shown that Adipose (fat) derived cell therapy can help people well into their 70s and 80s. It is minimally invasive, shown to be safe when using your own stem cells, and study after study shows that it can help patients by giving years of relief. The main drawback is that is expensive, ranging from $7000 and up depending on the joint and the clinic. Some clinics charges upwards of $30k or more. Then there is the problem of finding a reputable clinic that are experts at what they do and only treat those that research show can be helped. Physicians (MDs) are the only ones trained and allowed to perform micro-liposuction or bone marrow aspirations, so searching for stem cell treatments by a physician is the first place to start. Next, is to ask about their treatment approach and how they go about the procedure and why they use the approach that they do. Ask for research showing their specific treatment for your given condition. They should be able to corroborate. You can even use Google Scholar to research on your own. For example, type in “knee arthritis autologous stem cell therapy cartilage regeneration” in Google Scholar and you will get over 23,600 articles. You can narrow that down by searching for a systemic review or meta-analysis which combines the best studies and summarizes the results.
Now, Back To Surgery
1. Arthroscopy:
- Indicated for repairing or removing damaged cartilage, meniscal tears and tissues. Remember, they cant give back tissue. If you have a meniscal tear with decent cartilage volume, then the arthroscopy and clean up the meniscus and you may feel pretty good in the end. But remember, surgery is controlled trauma to the body for a specific reason. If you have cartilage loss that is causing symptoms, arthroscopy is not likely to yield much benefit. They can smooth the surface but just like when we have a rough piece of wood and sand it down to smooth it, we lose some of the wood. In fact, more recent research has shown that arthroscopy for arthritis has not led to improved outcomes and it is falling out of favor.
- Benefits include minimal invasiveness, but risks include infection and limited long-term relief.
2. Joint Replacement:
- Reserved for severe cases when conservative measures fail.
- Benefits include improved joint function, but risks include infection and the need for future revisions. 90% of replacements last >10yrs and 80% last up to 20 years. That is typically why orthopedists, generally, try to avoid replacing joints in younger patients. They will likely replace the replacement in younger patients.
- This is truly a last resort. As the saying goes, “Once you ring this bell, you cannot un-ring it.” You will live with the consequences. Even when successful, some patients were not aware of the limitations, such as pain with kneeling on the ground, scar tissue, range of motion issues, etc. Sometimes though, people wait too long. It is important to have a good orthopedist with which you can communicate and who will work with you to determine what your best course of action is given your imaging, symptoms, lifestyle, and health.
Conclusion: Empowering Yourself Against Knee Arthritis
Understanding and managing knee arthritis requires a multi-faceted approach. By incorporating lifestyle changes, exercises, over-the-counter treatments, and, when necessary, consulting with your physician for advanced options, you can take charge of your knee health. Remember, each person’s journey with arthritis is unique, so it’s crucial to work closely with your healthcare team to develop a personalized plan that suits your needs.
Wishing you the best on your journey to better knee health,
Andrew Pope MD